Abstract
Background. Targeted therapies have markedly improved overall survival (OS) outcomes in CLL patients. While significant racial differences in lymphoid malignancies have been reported, data on racial disparities in OS in the targeted therapy era are limited. We analyzed the SEER registry for patients diagnosed with CLL between 2009-2019 to explore the association between CLL cause specific death and race/ethnicity, sex, and socioeconomic status.
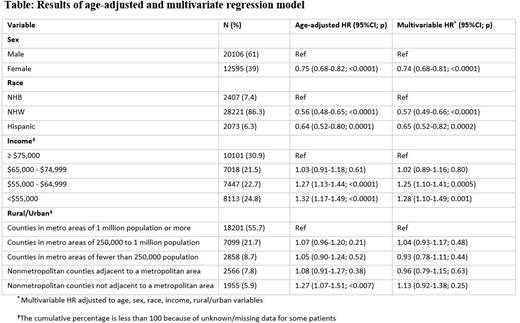
Methods. Patient characteristics and life tables were extracted from SEER for patients aged >15 years with a pathologically confirmed CLL (ICD-0-3) and diagnosed between 2009 and 2019. Variables extracted included: age at diagnosis, sex, ethnicity/race (non-Hispanic white [NHW], non-Hispanic black [NHB], Hispanic), annual household income (≥$75,000, $65,000-$74,999, $55,000-$64,999, <$55,000) and rural/urban area of residence. Multivariate Cox proportional hazard models adjusted for all variables were applied to calculate the hazard ratios (HR) of death due to CLL with corresponding 95% confidence intervals (CI). The assumptions of hazard proportionality and the interaction between the variables were tested.
Results. A total of 32,701 patients (61% males, 39% females) met the eligibility criteria and were included in the survival analyses (Table). The multivariate model adjusted for all covariates showed that OS was significantly better among women (HR=0.74; 95%CI=0.68-0.81), NHWs (HR=0.57; 95%CI=0.49-0.66), and Hispanics (HR=0.65; 95%CI=0.52-0.82) when compared to NHBs. OS was significantly lower in patients with annual income of $55,000-$64,999 (HR=1.25; 95%CI=1.10-1.41) and <$55,000 (HR=1.28; 95%CI=1.10-1.49) compared to income >$75,000. Income of $65,000-$74,999 did not show OS differences when compared to income ≥$75,000. Urban/rural residence was not associated with OS outcome.
Conclusions. In this registry-based analysis for CLL patients diagnosed in the era of targeted therapies, males, NHB patients, and patients with annual income <$65,000 had worse survival outcomes. In fully adjusted analyses, the risk of death in NHB patients was significantly higher when compared to NHW and Hispanics. NHB patients may have advanced disease staging at diagnosis, less access to targeted treatments, delays in treatment initiation, and different disease biology (biomarkers or genetic). Our study highlights the need to investigate the mechanism by which race/ethnicity interacts with disease prognostic factors and treatment factors that influence survival outcomes in CLL patients.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal